France launches new colon-cancer testing system for over 50s
France has a nationwide colon cancer testing programme aimed at 50-74 year olds, and now tests can be ordered online and done in the privacy of your own home.
Why should I test for colorectal cancer?
French health authorities recommend that if you are aged between 50-74, it is worth taking a colorectal cancer test every two years.
About 2.5 million people in France take this test every year.
90 percent of colorectal cancers which are picked up early can be cured.
Getting a test is completely free if you are registered with the French public health system. The test itself is painless.
How can I test for colorectal cancer?
On March 1st, the French government launched a new system whereby you can order a colorectal cancer test kit by post.
If you live in France and are between 50-74, you will likely receive a letter titled: Dépistage du cancer colorectal: un test simple et rapide qui peut sauver la vie
It looks something like the sample below:
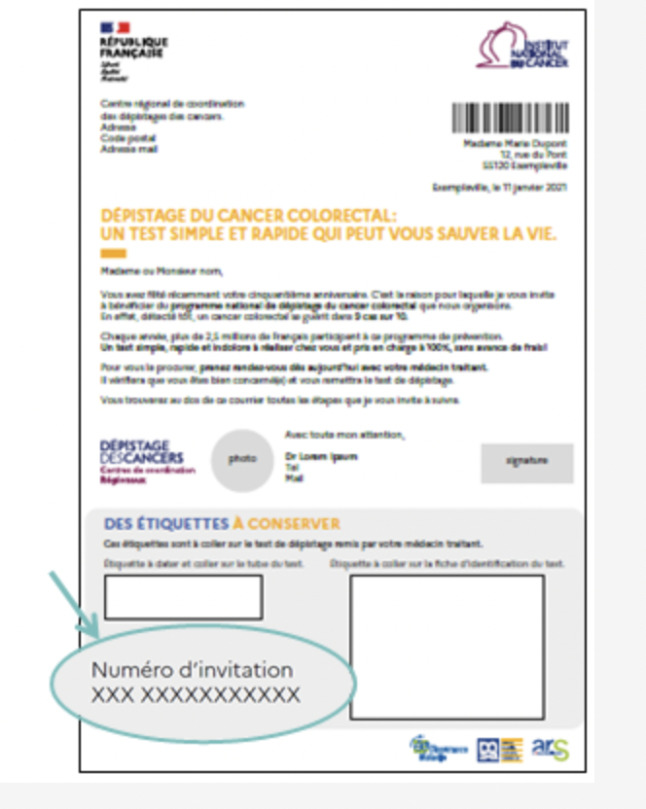
A letter inviting people to order a free colorectal cancer test kit. (Source: https://monkit.depistage-colorectal.fr)
Note the invitation number in the bottom left hand corner - you will need it to order the test online.
If you don't have a computer, you can also get a test kit following a consultation with:
- Your GP
- a gynaecologist;
- a gastroenterologist;
- a preventative care doctor recognised by the French public health system.
You complete the test at home following the instructions provided and then send it by post (a prepaid envelope is provided) to a lab for analysis. Your results will be available online three days after you send the test and you will receive confirmation fifteen days later in the post.
What if I don't receive a letter?
If you are aged between 50-74, you are supposed to receive a letter inviting you to get tested every two years, even if you don't display symptoms or don't have a family history of the illness. You will need to be fully registered in the French health system with a carte vitale in order to get the invitation.
If you don't receive one, you can contact your closest cancer testing centre - full list here.
What about other age groups?
If you are under 50 years old, you won't be sent a letter inviting you to take a test because you are not considered to be at risk of developing this cancer.
If you are over 74 years old, you will not be sent letters inviting you to get tested.
If you're not in this age group but you want a test, you can speak to your doctor to request one.
What if I test positive?
The vast majority of tests come back negative - and even if it is positive, this isn't a sure sign that you have cancer.
A positive test result means that blood has been detected in the sample. This could be a sign of cancer but could be something more benign.
If you receive a positive test result, your doctor will refer you to a gastroenterologist who will perform a colonoscopy to check whether you have colorectal cancer. In more than half of all cases, this colonoscopy reveals no signs of cancer.
Comments
See Also
Why should I test for colorectal cancer?
French health authorities recommend that if you are aged between 50-74, it is worth taking a colorectal cancer test every two years.
About 2.5 million people in France take this test every year.
90 percent of colorectal cancers which are picked up early can be cured.
Getting a test is completely free if you are registered with the French public health system. The test itself is painless.
How can I test for colorectal cancer?
On March 1st, the French government launched a new system whereby you can order a colorectal cancer test kit by post.
If you live in France and are between 50-74, you will likely receive a letter titled: Dépistage du cancer colorectal: un test simple et rapide qui peut sauver la vie
It looks something like the sample below:
Note the invitation number in the bottom left hand corner - you will need it to order the test online.
If you don't have a computer, you can also get a test kit following a consultation with:
- Your GP
- a gynaecologist;
- a gastroenterologist;
- a preventative care doctor recognised by the French public health system.
You complete the test at home following the instructions provided and then send it by post (a prepaid envelope is provided) to a lab for analysis. Your results will be available online three days after you send the test and you will receive confirmation fifteen days later in the post.
What if I don't receive a letter?
If you are aged between 50-74, you are supposed to receive a letter inviting you to get tested every two years, even if you don't display symptoms or don't have a family history of the illness. You will need to be fully registered in the French health system with a carte vitale in order to get the invitation.
If you don't receive one, you can contact your closest cancer testing centre - full list here.
What about other age groups?
If you are under 50 years old, you won't be sent a letter inviting you to take a test because you are not considered to be at risk of developing this cancer.
If you are over 74 years old, you will not be sent letters inviting you to get tested.
If you're not in this age group but you want a test, you can speak to your doctor to request one.
What if I test positive?
The vast majority of tests come back negative - and even if it is positive, this isn't a sure sign that you have cancer.
A positive test result means that blood has been detected in the sample. This could be a sign of cancer but could be something more benign.
If you receive a positive test result, your doctor will refer you to a gastroenterologist who will perform a colonoscopy to check whether you have colorectal cancer. In more than half of all cases, this colonoscopy reveals no signs of cancer.
Join the conversation in our comments section below. Share your own views and experience and if you have a question or suggestion for our journalists then email us at [email protected].
Please keep comments civil, constructive and on topic – and make sure to read our terms of use before getting involved.
Please log in here to leave a comment.